What is Papular Dermatitis? Causes, Symptoms, and Treatments Explained
Introduction
Ever noticed itchy, red bumps on your skin that seem impossible to ignore? If yes, you might be dealing with a condition called papular dermatitis. It’s not just a fancy term for regular skin irritation—it’s a specific condition that affects many people. Understanding what papular dermatitis is and how to manage it can be a game-changer for your skin health. Let’s dive into the causes, symptoms, and treatments that can make a real difference.
What is Papular Dermatitis?
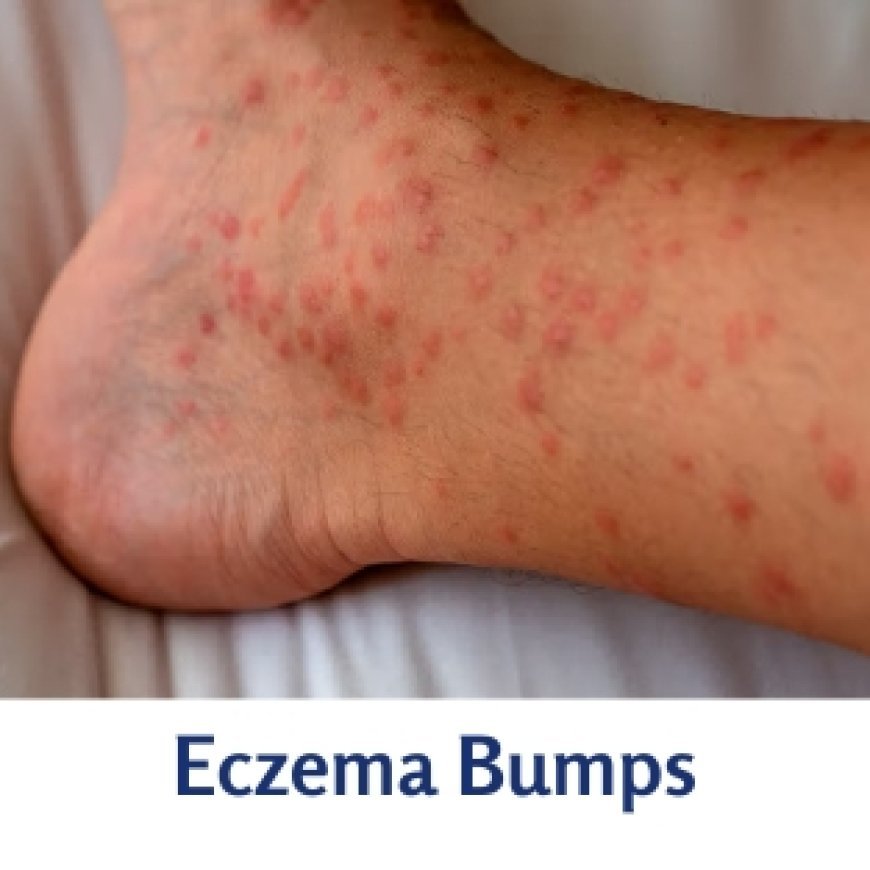
Papular dermatitis is a skin condition characterized by small, raised, red bumps (papules) that are often itchy and inflamed. Unlike other skin conditions like eczema or psoriasis, papular dermatitis focuses on the formation of these distinctive bumps. While it might sound alarming, the condition is manageable with the right knowledge and care.
Causes of Papular Dermatitis
Environmental Factors
Your environment plays a significant role in triggering papular dermatitis. Common allergens like pollen, dust mites, or even harsh chemicals in cleaning products can irritate your skin. Weather changes, especially dry or humid conditions, can also worsen symptoms.
Genetic Predisposition
If skin issues run in your family, you’re more likely to experience papular dermatitis. Genetics influence your skin’s sensitivity and how it reacts to irritants.
Lifestyle Factors
Your daily habits matter too. A poor diet lacking essential nutrients can weaken your skin’s barrier. Dehydration and irregular personal hygiene routines also contribute to flare-ups.
Symptoms of Papular Dermatitis
Physical Symptoms
The most noticeable signs are the small, red bumps that appear on your skin. They’re often accompanied by redness, swelling, and an intense urge to scratch. Scratching, however, can lead to secondary infections, so it’s best avoided.
Psychological Impact
Living with visible skin issues can take a toll on your mental health. Feeling self-conscious or stressed about your appearance is common but can be managed with support and self-care.
Diagnosing Papular Dermatitis
Medical History
Your doctor will start by asking about your symptoms and triggers. Be prepared to share details about your skincare routine and any products you use.
Skin Tests
Patch testing is a common method to identify allergens causing your condition. Other diagnostic tools might include examining your skin under a microscope.
Treatments for Papular Dermatitis
Topical Treatments
Using a fragrance free cream is one of the best ways to soothe irritated skin. These creams are gentle, hydrating, and reduce inflammation without adding unnecessary irritants. Corticosteroid creams may also be prescribed for more severe cases.
Lifestyle Adjustments
Avoiding known triggers, like specific soaps or fabrics, can prevent flare-ups. Establishing a gentle skincare routine with hypoallergenic products makes a world of difference.
Home Remedies
Natural options like aloe vera or oatmeal baths can calm your skin and reduce itchiness. Regular moisturizing is also crucial for maintaining healthy skin.
Medical Interventions
For severe cases, dermatologists may recommend advanced treatments, including immunotherapy or prescription medications. Regular follow-ups ensure your condition remains under control.
Preventing Papular Dermatitis
Skin Care Routine
Choose mild cleansers and moisturizers to keep your skin healthy. Avoid over-exfoliating, which can irritate your skin.
Environmental Precautions
Minimize exposure to allergens by using air purifiers and wearing protective clothing in harsh weather conditions.
Healthy Lifestyle Choices
A balanced diet rich in vitamins and antioxidants supports overall skin health. Managing stress through activities like yoga or meditation can also reduce flare-ups.
Myths and Facts About Papular Dermatitis
Common Misconceptions
Some believe papular dermatitis is contagious, but it’s not. Others think it’s a permanent condition, but with proper care, symptoms can be managed or even resolved.
Evidence-Based Facts
Research shows that identifying and avoiding triggers is the most effective way to prevent flare-ups. Additionally, using fragrance free cream regularly can significantly improve symptoms.
Living with Papular Dermatitis
Coping Mechanisms
Building confidence despite visible symptoms is essential. Connecting with support groups can provide emotional relief and practical advice.
Long-Term Management
Consistency is key. Stick to your skincare routine and consult your dermatologist for adjustments when needed.
Conclusion
Papular dermatitis might be annoying, but it’s far from unbeatable. By understanding its causes and symptoms, you’re better equipped to manage it. Whether it’s using a fragrance free cream, adopting a new routine, or seeking medical advice, taking action today can lead to healthier, happier skin tomorrow.
FAQs
1. What is the difference between papular eczema and eczema?
While both conditions involve inflammation, papular eczema is marked by small, raised bumps, whereas eczema often causes patches of dry, flaky skin.
2. Can papular eczema go away on its own?
In some mild cases, it might resolve without treatment, but most people need skincare adjustments or medical intervention.
3. Are there any dietary restrictions for managing papular eczema?
A diet rich in fruits, vegetables, and omega-3 fatty acids supports skin health, but specific restrictions depend on individual triggers.
4. How often should I use fragrance free cream for papular eczema?
Apply it at least twice daily or as recommended by your dermatologist to keep your skin hydrated and calm.
5. Can stress worsen papular eczema symptoms?
Yes, stress is a known trigger for many skin conditions, including papular eczema. Managing stress can help reduce flare-ups.
What's Your Reaction?